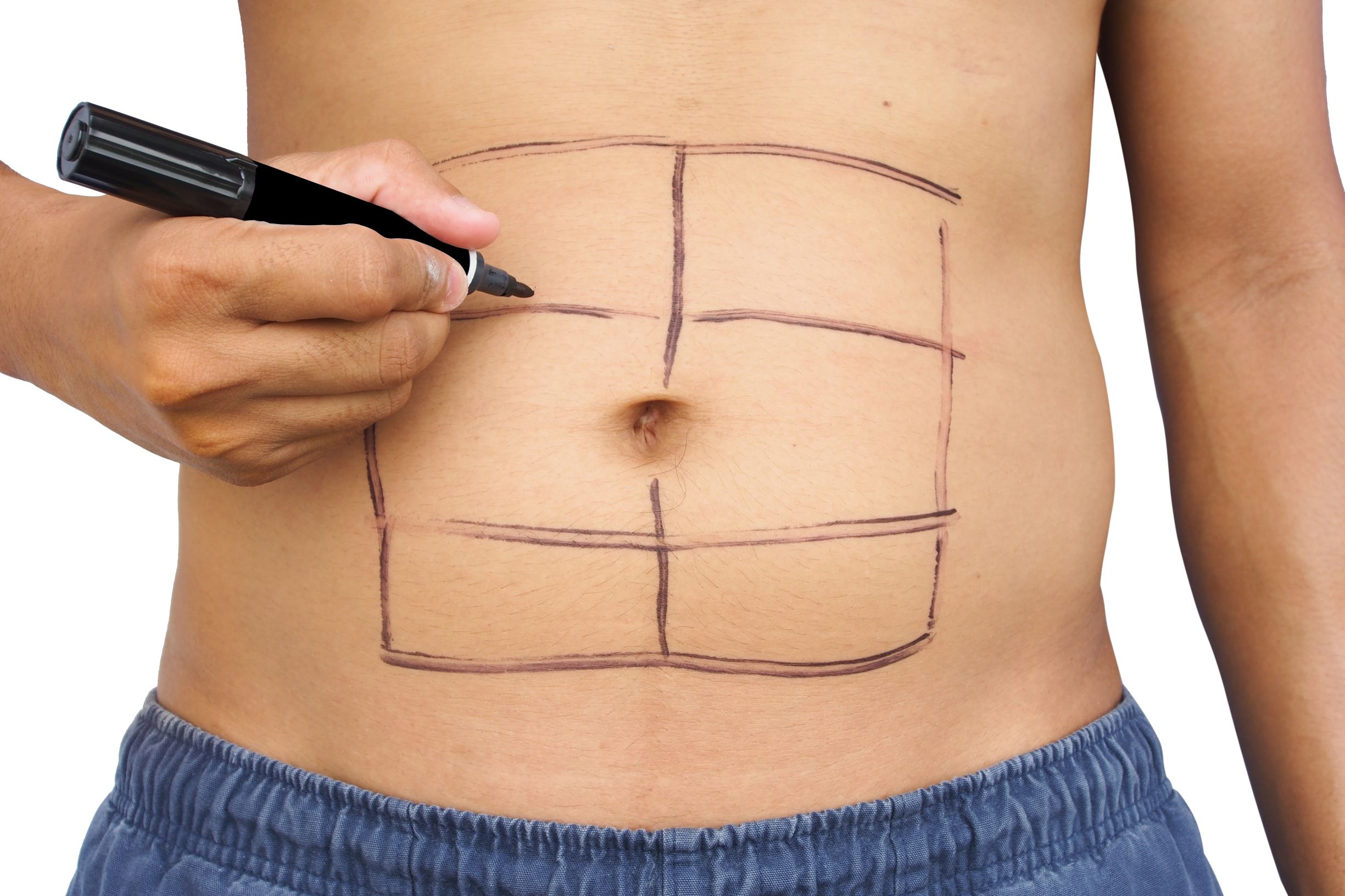
The terms “core strength” and “spinal stabilization” often invokes the image of ripped six-pack abs and trimmed obliques. Although the rectus abdominis (6 pack muscle) and the obliques serve important roles in generating efficient movement of our bodies, in isolation they do not serve as effective stabilizers of the spine. Instead, those muscles must work in dynamic coordination with other muscles to provide spinal protection and “core strength”. If you don’t know these muscles, don’t worry, we will introduce you to them below! Core function and spinal stabilization are broad topics that cannot be covered in a single blog. In this series of writings, we plan to explore both of these topics in relationship to our approach to physical therapy, Functional Manual Therapy ™. The intention of this article is to provide you with a functional context of how our core functions and how our posture impacts core function.
An Optimally Functioning Core Efficiently Generates and Regulates Intra-Abdominal Pressure
A helpful model to view our core as a pressure regulation system is to visualize a cylinder, like a closed can of soda. This model was initially discussed by Mary Massery, a fellow physical therapist and renowned researcher. As long as the can remains sealed, the pressure contained within the can increases the structural integrity of the otherwise thin and weak aluminum walls. In this case, the can withstand compression, twisting and shear forces without damage. However, when you break the seal and lose pressure, the structure fails and can easily be crushed.
Key “Can” Muscles
When we look at the above model, the glottis is the top seal. The glottis is located at the top of your windpipe and houses your vocal cords.
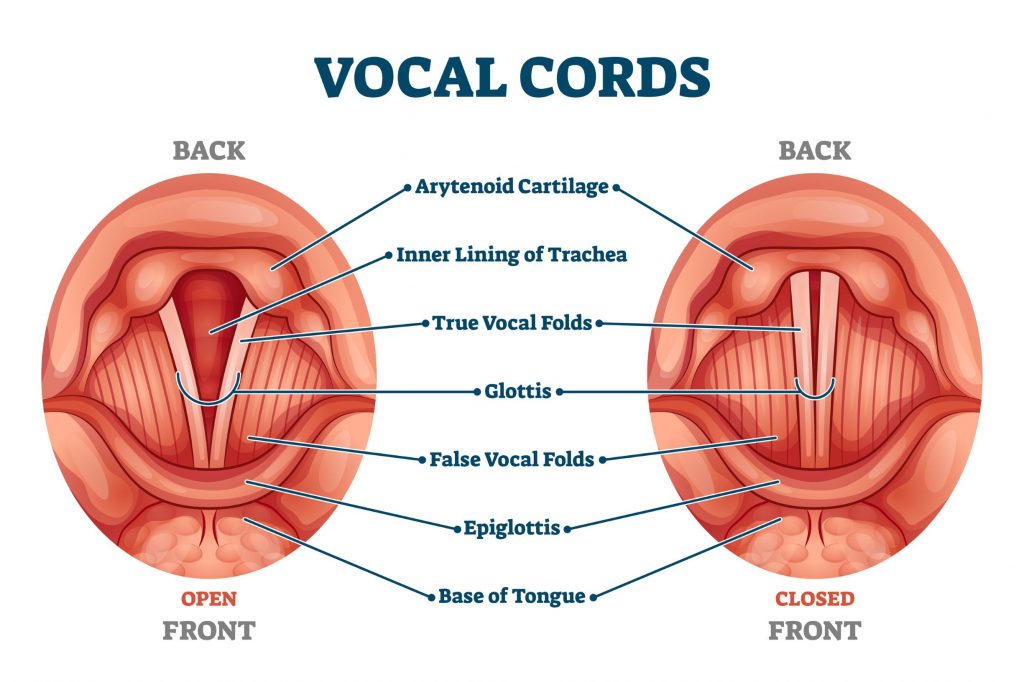
Say “ahh” – those are your vocal cords regulating the rate of pressure escaping from your chest while simultaneously vibrating between 100-1,000 cycles per second to create the desired tone. Amazing!
The glottis is dynamic in its role as a pressure regulator. It can be completely closed when you bear down, which allows no air to escape and provides maximal pressure within your throat, chest, and abdomen. This increased pressure provides a stable structure for maximal force production and structural integrity. An example of this is when a powerlifter exerts maximal effort to lift a very heavy object or move an object very quickly. Max pressure within the confines of your head, chest, and abdomen allows you to create maximal force, however, you can’t hold this pressure for long because you will push all the blood to your head and pass out. This is technically called a “Valsalva maneuver” in case you are familiar with that term.
Rather than just being open or closed, the glottis can regulate intra-abdominal pressure by slowly releasing pressure to match the desired force production. The most effective and safe way to produce this pressure is to slowly exhale during the execution of maximal effort. In an efficient system, the glottis acts as a valve that precisely regulates the amount of pressure that is required for the task you are performing. When we want high pressure (without blacking out) we find strength by bearing down for short periods while simultaneously exhaling slowly.
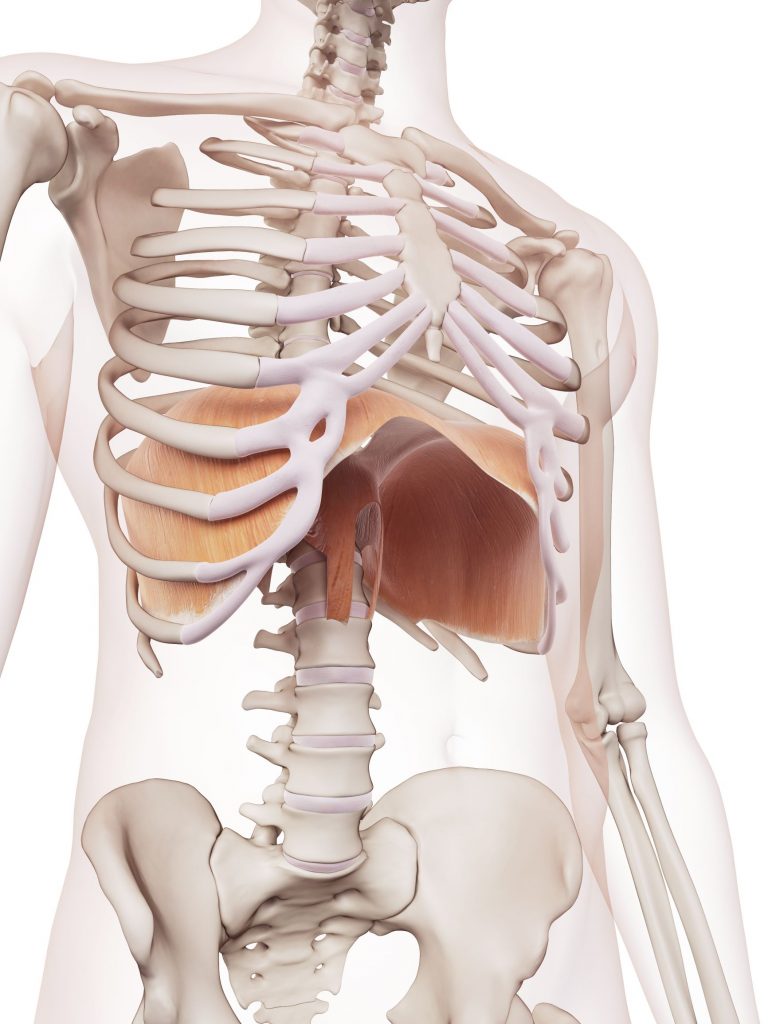
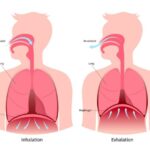
Cleary, the glottis plays an important role in the function of our core, but the glottis does not work alone to regulate these pressures. It must work in coordination with another muscle at the bottom of our rib cage to generate pressure in our trunk. That muscle is the diaphragm. The diaphragm is a dome-shaped muscle that lies in the middle of your ribcage. It has 2 primary functions, breathing and pressure creation. When the diaphragm contracts it pulls air into the lungs. The diaphragm contraction pushes the muscle downward and compresses the abdominal organs increasing the pressure in the abdomen. This pressure pushes out in all directions. The goal of our abdominals, back and pelvic floor muscles is to not let this pressure escape, and therefore increase stability through intra-abdominal pressure.
The pelvic floor opposes the contraction of the diaphragm and acts as the seal on the bottom of the can. If the bottom of the can doesn’t work, you either pee or poo when you don’t want to, or your guts fall out (prolapsed organs are real and you don’t want one). On a less extreme note, we know when the pelvic floor doesn’t work as it should, neither do our back stabilizing muscles. A week pelvic floor absolutely equals a weak core.
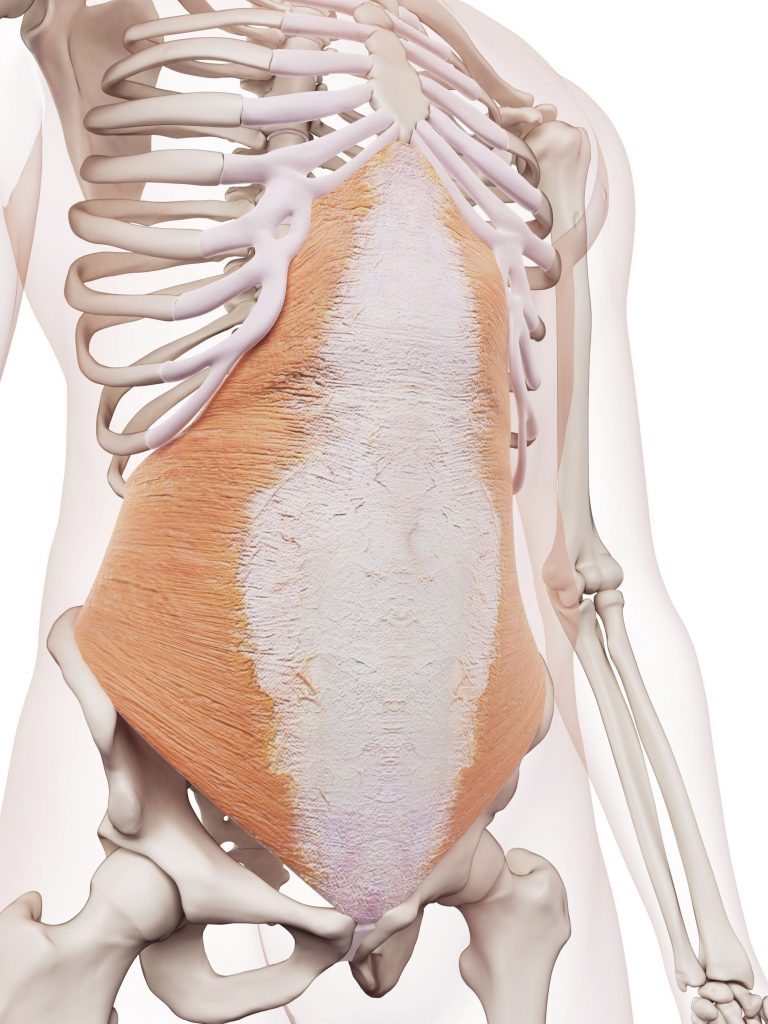
The transverse abdominis, internal and external obliques, and parts of the quadratus lumborum all act as the walls of the canister, and actively contract to resist the pressure created by the diaphragm moving downward. If these walls are weak, or have structural breaks, the intra-abdominal pressure is lost and the structure can fail (like the soda can). Failure of these walls can result in many things including hernias, where part of your intestine can push through the abdominal wall. Commonly this occurs around the belly button or groin.
Transverse Abdominis 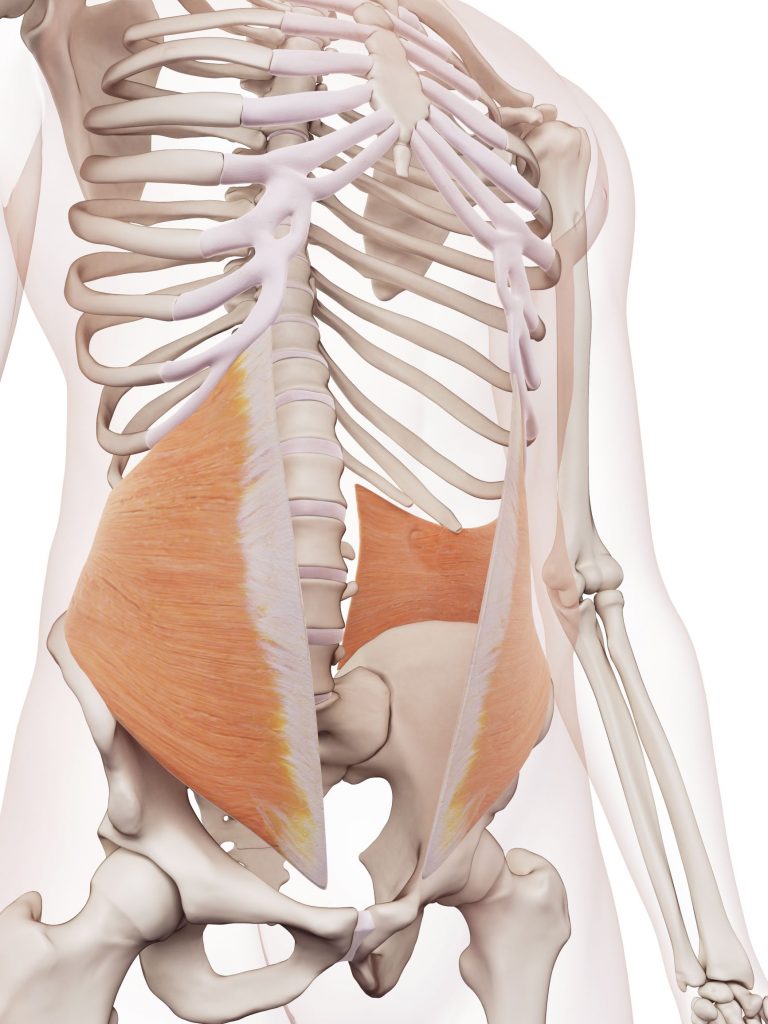
Internal Oblique 
Quadratus Lumborum
Failure of the abdominal wall can also result in diastasis recti, a condition where the abdominal wall is stretched thin resulting in separation of the rectus abdominis. In men, this occurs most often between the ribcage and the belly button and in women between the pubic bone and the belly button (this commonly occurs during pregnancy).
The deep fibers of the psoas, multifidus muscles, parts of the quadratus lumborum, and other very small muscles between each of the spinal vertebrae work in conjunction to stabilize the innermost load-bearing structure, the spinal column. Simply put, they are like bolts that hold a tall building together. If a bolt breaks, the building loses part of its structural integrity and can fall apart. The contraction and strength of these deep muscles are enhanced by the presence of intra-abdominal pressure, therefore these small and larger muscle groups are dependent upon each other for optimum function. We will discuss the function of these deep core muscles in our next blog post.
The pressure maintained within our trunk is a dynamic anchor that serves as a base of support for our limbs to move as well as distribute the forces affecting our bodies in static and dynamic tasks.
The effectiveness of pressure regulation is dependent on mechanical, neuromuscular and motor control components (see future blog posts on this topic). From a neuromuscular perspective, alignment of the structure has a direct impact on the function on an individual or a group of muscles. Yes, posture and alignment DOES matter!
Optimizing alignment and dynamic control of your skeleton while breathing (see Dr. Rumford’s blog “Get Over Yourself” and “Guide to Optimal Sitting Posture” for a more detailed discussion) should be the primary goal for optimal performance. Our postural strategies play a pivotal role in the physics of our muscle groups and therefore pressure regulation.
Muscles function a lot like Goldilocks and The Three Bears. If a muscle is too short (papa bear) or too long (mama bear) it loses strength. However, if the length of a muscle is just right, it can generate peak force.
Now think about the core cylinder up above and apply this same concept to muscles of our core. The diaphragm, pelvic floor, all the walls, all have an ideal resting length where they can generate the most effective contraction to regulate pressure.
These are examples of common dysfunctional postures with the last being fairly efficient where skeletal alignment is maintained and the pressure from gravity moves evenly into the base of support. When you observe the dysfunctional postures, picture the core cylinder and how the muscle lose their optimum length/tension relationship. In postures 1-3, the structure is compressed, lengthened, twisted or sheared, and therefore pressure retention is compromised simply because the structure is positioned poorly.
The pressure in our abdominal cavity gives buoyancy to our structure so no one piece of the structure is adversely loaded. When our alignment shifts away from optimum and our pressure system is compromised we are more likely to develop mechanical stress points (disks, joints, ligaments, etc.). From this compression the mechanical stress points break down (arthritis, tendonitis, etc.), and as damage accumulates we inherently become more and more stiff.
Clinically we see the closer the body gets to being efficiently aligned the stronger the patient becomes. So posture is absolutely important from the standpoint that efficient alignment gives you the best opportunity to access your pressure system and therefore your core strength. When posture is aligned and balanced with weight distributed into the base of support, there is a natural contraction of your core muscles – we call this an Automatic Core Engagement™. When we learn to utilize efficient postural strategies, we naturally strengthen our core and can more optimally train our “mover muscles” to perform the necessary tasks.
So take some time to observe your posture and your breathing habits. How do you stack up relative to posture 4 above? Are you feeling stiff and locked into your posture? If getting vertical feels impossible to achieve or maintain, you are working against too many variables to have success. Some of these barriers are mechanical stiffnesses and some reflect that your brain physically doesn’t know how to achieve these postures and needs to be guided. This is the job of a Functional Manual Therapist™ and we specialize in helping people achieve a more optimum state of function. Reach out and enquire about how we can partner with you to help you Achieve Your Potential™.