Menopause is something we hear a lot about, but do we actually know and understand the changes that are happening in the female body during this time period? Menopause is defined as a 12 month period where women experience no bleeding. The average age of menopause is 51 years old. Prior to that, women can experience all kinds of symptoms for up to 7-8 years before finally arriving at menopause. This period leading up to menopause is called perimenopause.
Common symptoms present during perimenopause and menopause include:
- Hot flashes
- Mood alterations
- Night sweats
- Sleep disturbances
- Weight gain (usually in the abdomen)
- Brain fog
- Low libido
- Vulvo vaginal atrophy / Genitourinary syndrome of menopause
- Irregular periods of length and timing
- Changes in hair and skin
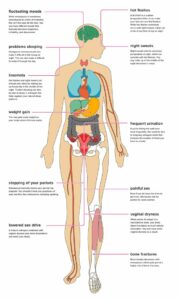
The average age for peri-menopause is 47.5 years old. Currently, the average life expectancy for women is 81 years of age which means some women are spending half their lives experiencing these symptoms! Although rare, menopause can occur prematurely in about 5% of women between the ages of 40 and 45 and 1% before age 40. It can also occur after surgery to remove the uterus (hysterectomy) and / or ovaries (oophorectomy).
To better understand why changes occur during perimenopause and menopause, let’s first talk about what happens during menstruation.
The endocrine system in the body is made up of glands that talk to each other to release hormones. The hypothalamus signals to the pituitary gland to release FSH (follicle stimulating hormone). FSH then stimulates the ovaries to produce follicles which contain an immature egg. FSH also stimulates the uterus to start increasing blood supply and endometrial lining. As the follicles mature, there is a surge of estrogen. The rising estrogen levels then stimulate another hormone to be released called LH (luteinizing hormone). LH then stimulates ovulation to occur. After ovulation, there is a surge of progesterone. If sperm is present, a woman may become pregnant. If not, the egg and endometrial tissue is shed and menses starts.

One of the first hormonal changes to occur during perimenopause is a decrease in inhibin levels. The ovaries make inhibin which tells the pituitary gland to make less FSH. During perimenopause and menopause, inhibin levels decrease which causes FSH levels to increase and a consequential decline of estrogen. Menstruation becomes irregular as a result of fluctuations in FSH and estrogen levels. Progesterone levels also decrease. The drop in estrogen levels is what causes the symptoms of perimenopause and menopause.
A pelvic health physical therapist can help women with a number of the symptoms of perimenopause and menopause.
- Vulvo vaginal atrophy / Genitourinary syndrome of menopause – This can include vulvar and vaginal dryness and itching, pain with intercourse, burning / soreness, pelvic floor tightness, feelings of recurrent UTI’s with negative culture, or recurrent UTI’s. Oftentimes the urethra may appear open or gaping which puts individuals at higher risk for UTI’s. Pain with initial penetration during intercourse may also occur due to dryness.
- Prolapse – Prolapse is when one of the pelvic organs descends down towards the vaginal opening. It can worsen in menopause due to the decrease in estrogen. As this occurs, there’s less bulk to the vaginal tissue allowing for greater ease of organs to descend through the vaginal walls. Working with a team of health care providers can be beneficial for the decrease in progression and management of prolapse.
- Incontinence – Stress urinary incontinence is when leakage of urine occurs with an increase in intra-abdominal pressure (laughing, sneezing, coughing, jumping). This can also occur or worsen in menopause as there’s less closure of the urethra.
- Hot flashes and night sweats – Ovary function is important to hormone balance particularly estrogen and progesterone. Ovaries can get bound down by fascial or soft tissue restrictions which can limit their ability to fully function. Visceral (organ) mobilization especially to the ovaries improves mobility of this organ and thus in its ability to function well.
Typical treatment for these diagnoses include medications and living with it. This doesn’t have to be the case! Pelvic health physical therapy and the Functional Manual Therapy approach can help improve blood flow to the pelvis through manual therapy to adjacent organs, veins and arteries, joints, and soft tissue. Visceral (organ) mobilization improves mobility and functionality of the pelvic organs which in turn can help with some menopausal symptoms like hot flashes and night sweats. Functional Manual Therapy addresses postural dysfunction and improves initiation, strength, endurance, and motor control of core muscles including the pelvic floor. This will help with better management of pressure systems of the body.
If you or a loved one struggles with perimenopausal / menopausal symptoms, know that you are not alone. We’re here to help. If you are experiencing the aforementioned symptoms and want to reduce your symptoms, contact us today for an evaluation and treatment.