Detailed Description of the Current Problem
We need to know your story. Help us understand exactly what is going on in your current presentation by offering insights into the following information, starting with:
What do you believe was the initial mechanism(s) that initiated your current situation?
- This could be a fall, trauma, or an action that was being performed that correlates with the onset of your symptoms.
- Sometimes what caused your problem is an obvious event, however in many cases patients have a difficult time identifying any mechanism.
- Please be aware that your pain should make sense. If there was not an obvious event that started the pain, then the pain may be a combination of factors, including:
- Activities performed repetitively in a stressful manner
- Physiological factors such as low vitamin/mineral levels, mold / environmental toxin exposure
- Autoimmune conditions
- Etc..
Key factors for symptom reporting
Please describe the symptoms you’re experiencing to the best of your ability. The nature of how it feels can give clues to the tissue(s) that are symptomatic. We encourage you to take notes and bring them to your appointment. Below are some of the key factors that help us best understand your experience of symptoms, and more quickly get to the root cause of your problem.
Location – Where are your symptoms located?
- The more specific the better, as small differences in locations can indicate dramatically different anatomical causes. If you have symptoms over a large area, try to identify different epicenters.
- If you have multiple locations of pain/symptoms, try to rank them in the order of importance to you. Which one would you get rid of first if you could choose?
- Are your symptoms easy to describe or more vague and hard to describe?
- Do the symptoms feel specific and localized? Or do they spread to other locations in the body?
- Do the symptoms feel connected or isolated in nature?
Intensity – How severe are the symptoms?
- We believe that minor symptoms warrant investigation. Intensity of symptoms can be variable based on several factors including: illness, inflammatory levels, and duration of symptoms Symptom intensity is also influenced by previous experiences with pain and levels of impact to quality of life.
- When completing a visual analogue scale (scale of 1-10) for your symptoms be honest with your ranking of pain. Zero is truly zero, no symptoms. Ten out of ten is the worst pain imaginable, and it can’t get worse. Do not understate or over-embellish, so that we can better appreciate the impact the symptoms are having on you.
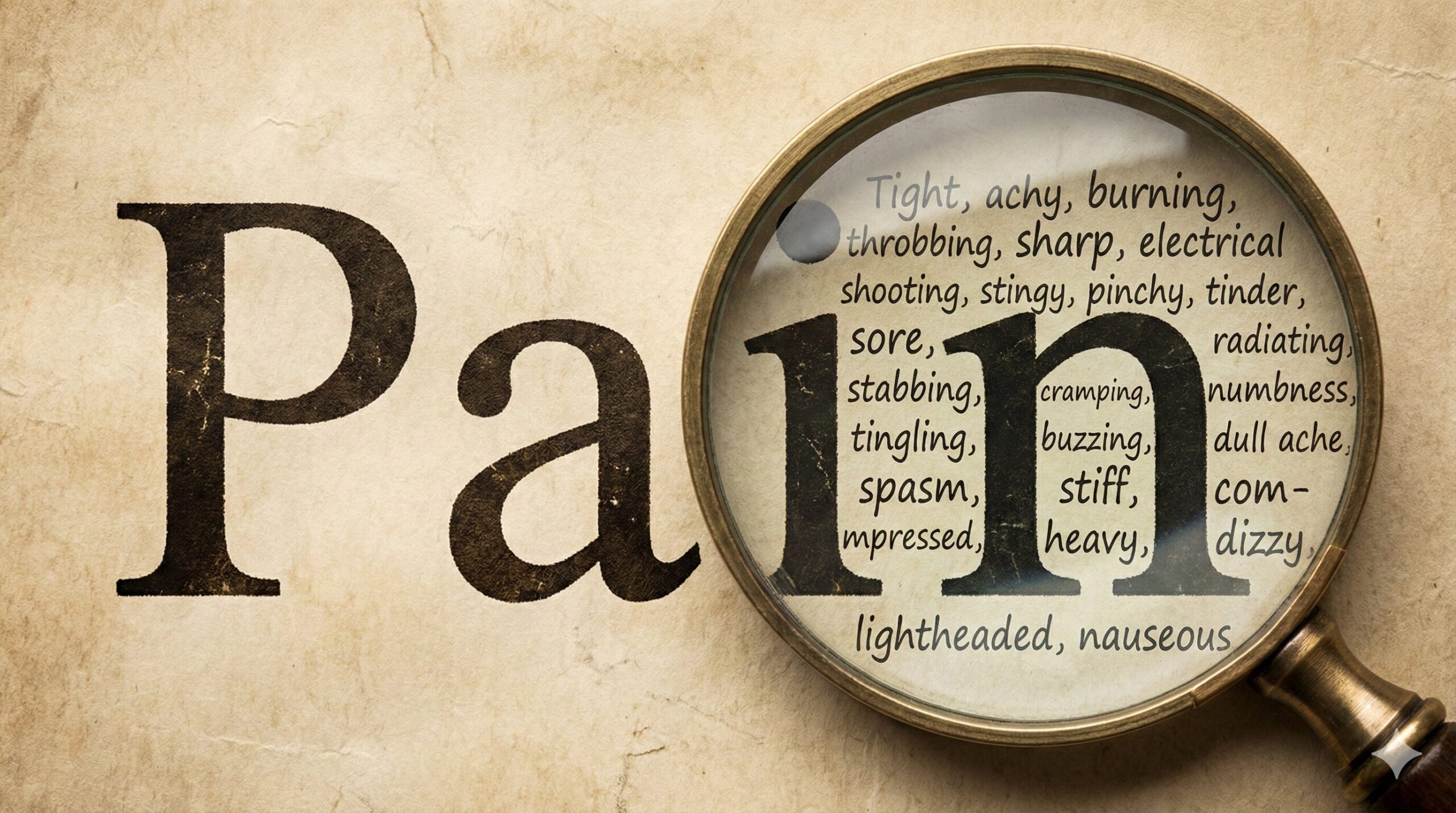
Quality – What type of symptoms are you experiencing?
- Below is a list of some common words used to describe physical symptoms. This is not an exhaustive list, but it can be used to help get started with describing the sensations you are feeling:
- Tight, achy, burning, throbbing, sharp, electrical shooting, stingy, pinchy, tinder, sore, radiating, stabbing, cramping, numbness, tingling, buzzing, burning, dull ache, spasm, stiff, compressed, heavy, dizzy, lightheaded, nauseous, etc.
- Are the symptoms experienced as shallow vs deep?
- If these descriptors do not apply, can you describe it in terms of shape or color? What description works best for you?
- By having workable descriptions, the therapist is able to open a dialogue with you to judge how things are progressing rather than simply asking “how are you feeling?”
What makes it better or worse? – Even if symptoms are always present, what
- Even if symptoms are always present, we need to know what makes it better or worse. Think about it this way, if you could be paid a million dollars to make your symptoms worse (or more intense), what would you do to guarantee you would increase your symptoms? (We know, this is a weird mind game, but it really does help us better understand your symptoms.)
- Then think about it the same way with decreasing your symptoms, even a subtle reduction in symptoms can help us more quickly find the path to resolution.
- For example: walking helps your pain, but standing increases your symptoms. How long can you stand or do the activity before symptoms start?
- If you change position or activity, do symptoms persist or do you get relief? As you rest, do symptoms return, but are different from those in the standing example?
- Is your pain lessened by ice, heat, and/or NSAIDS (anti-inflammatory medications)?
- Does it hurt to sit? If so, how long before symptoms start? How is the transition out of sitting?
- Once standing do you get relief or does it just change?
- Have you tried any therapeutic movement strategies?
- Have you tried physical therapy, massage, chiropractic or other modalities such as acupuncture?
Daily Trends – Map your symptoms over a 24 hour period of time
- As providers we expect your symptoms to change from visit to visit – and a 24 hour timeline is our first baseline.
- Are your symptoms different in the night time, compared to when you first wake up? How do they change throughout the day?
- What motions are most provocative, and are these more provocative in the morning vs the evening?
Night time symptoms are very important
- Does the pain keep you from falling asleep? Does the pain wake you up at night? What time? Can you reduce the pain by changing position or using props for support?
- Does the pain feel vague or specific? Do the symptoms feel as if they are within you and three dimensional or more specific to the skeleton?
- Have you tried sleeping in another bed, and does that impact your symptoms?
- What motions are you most sensitive to in the morning?
- Example: The morning is stiff, achey, perhaps vulnerable. Looser with movement, but worse as the day progresses. This often reflects inflammation and a response to the cumulative stress of the day.
Trauma History
- Past injuries or traumas – Car accidents, falls, surgeries, ankle sprains, shoulder injuries (big or small) are important things to share. We will prioritize what makes sense.
- It is very common, as we assess and treat areas of the body, that patients will recall a trauma that was absent from the initial discussion. This reflects the concept that ‘the body keeps the score’ when it comes to trauma and stressors that affect your overall wellness.
- Areas impacted by trauma become disconnected from the body as a whole and grossly impact both your ability to move and the ability to perceive movement or proprioception. If you can’t feel it, you can’t move it. If we have impaired sensory awareness, those areas tend to be more painful.
- All past surgical interventions – should be included. This includes: C-sections, ablations procedures, appendectomies, tube ligations, wisdom tooth extraction, etc.
- Do you have any internal medical devices, such as an IUD? Staples, clips or mesh supports? Pacemaker?
State of Mind
- Do your symptoms increase with life stresses that are not physical? For example, does your pain increase when you are under emotional stress? Are you inclined to push through the pain or do you adopt strategies to mitigate the symptoms?
Illness or systemic relationships
- Do your symptoms increase or change based on your dietary intake? Are you prone to digestive tract irritation, GERD, food intolerances? Do you associate changes in your musculoskeletal pain with alternative system dysregulation?
- Genetics can play a big role. Have you been diagnosed with a connective tissue disorder, autoimmune disorders, MAST cell problems?
Imaging or Medical Diagnostics – MRIs, x-rays, EMG studies, etc.
- Imaging is very useful as a part of the information gathering process. It is important to keep in mind, though, that imaging does not tell the full story. The combination of your history, a thorough physical exam, and your imaging findings will help determine the appropriate diagnosis and prognosis.
- Our software is often not compatible with disc drives given to patients. Printed reports will be added to your file.
Do you have a primary care provider?
- When was the last time you had a physical?
- Please provide the name and office of your provider so we can be in direct communication with them regarding your case.
Path to Healing
As you can see, we are very interested in knowing as much about you as possible. It is also helpful to go through this process of knowing your symptoms as a patient, especially if you have symptoms that have lasted longer than 3 months.
It can be hard to recognize change if you have been in pain for long periods of time, and some changes to date time. If we can help the brain recognize change, celebrate wins, we accelerate your neuroplastic brain changes by reinforcing the desensitization of the neural pathways. Reference your baseline over the course of weeks or months to establish pattern recognition of difference.
If you have difficulty answering some of the questions with any sort of specific certainty, a journal can help you track symptoms and identify trends and patterns.
We look forward to having you in the office and patterning your path to recovery, let’s thrive together!