March is Endometriosis Awareness month. This pelvic pain diagnosis is one that’s near and dear to my heart. I not only treat this diagnosis since I specialize in pelvic health but I was officially diagnosed with endo last year. Let’s talk about what endo is and isn’t, signs and symptoms, how it’s diagnosed, and management options.
Endometriosis affects 10-15% of all women of reproductive age and 70% of women with chronic pelvic pain. It occurs when cells similar to those that line the inside of the uterus are present outside of the uterus. There are many definitions out there that describe endo lesions as endometrial lining that ends up outside the uterus and this just isn’t true. These cells can end up within the pelvic cavity – on the ovaries as cysts, fallopian tubes, pelvic wall, and behind the uterus and in front of the rectum (anatomical term – pouch of Douglas). In other instances, these cells can be present outside the pelvic cavity – intestines, lungs, diaphragm, and in rare cases, the brain. When these cells are exposed to inflammation, it sets off a cascade of effects to create more inflammation (which further feeds this cycle). These cells also create their own nerve and blood supply, and thicken to form dense scar tissue or adhesions. This scar tissue can distort anatomy which may contribute to pain with intercourse and pain with bowel movements. The amount of inflammation present in the system can also contribute to pain in the pelvis as well as other areas of the body. Endometriosis can be extremely painful and can affect quality of life for many individuals.
Notice how estrogen and hormones haven’t been brought up yet? At its core, endometriosis is an inflammatory driven disease state. Although it’s quite common to have high estrogen with endometriosis, not everyone does. It’s still important to check hormone levels but shifting the lens in which endometriosis is looked at is important in order to better understand it.
So the big question – why is this happening? Where do these cells even come from and how do they end up where they end up? The unfortunate answer is, we don’t know. Research has shown that mothers exposed to dioxins (an environmental pollutant) during pregnancy can contribute to their daughters having an increased likelihood of developing endometriosis. For many years, there was the theory of retrograde menstruation being the cause of endometriosis. Although retrograde menstruation may contribute to menstrual pain, it doesn’t explain how some individuals have endometrial lesions present at birth.
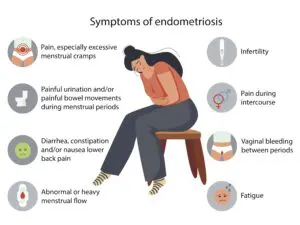
More commonly known symptoms of endometriosis:
- Painful, heavy periods (often times with clots present)
- Pelvic pain throughout menstrual cycle (can be during ovulation, can be any other time of the cycle)
- Low back pain
- Constipation or diarrhea
- Digestive issues
- Pain with intercourse
- Infertility
- Nerve pain down legs
- Severe bloating
- Nausea / vomiting
- Pain with bowel movements
- Urinary urgency / frequency (may have pain associated with voiding)
- Headaches
- Brain fog
- Fatigue
- Depression
Not as known symptoms of endometriosis:
- Cold or flu like symptoms throughout your cycle
- An increase in other musculoskeletal pain around menstruation
- Difficulty breathing
- Heart palpitations
- Rib and diaphragm pain, shoulder or neck pain
- Lung collapse
- Rapid heart rate
This is not an all encompassing list. The severity of pain differs from person to person. Some individuals with endo are asymptomatic. Reading through this list, look at how many symptoms don’t have anything to do with the pelvis! Remember, endo is not just a uterine disease. It’s a systemic disease that can affect multiple body systems.
Diagnosis:
The gold standard for diagnosing endo is laparoscopic surgery. This is done to visualize and better understand the full extent of the disease for proper staging. Getting a diagnosis can be incredibly powerful for individuals to finally get answers to their pain, to understand why they haven’t been able to conceive if they’ve been trying, and to know going forward how they can better manage their symptoms. Ultrasound may show lesions or cysts present on the ovaries or deeply infiltrative lesions however ultrasound won’t always visualize superficial lesions. Superficial lesions can still cause immense amounts of pain. Some OB’s may use an MRI or CT scan to visualize the pelvic region but those won’t necessarily show superficial lesions either.
Symptoms Management:
- Excision vs ablation surgery: During excision surgery, the surgeon goes in and cuts out or excises the endometrial lesion and the surrounding tissue to ensure the entire lesion is taken out. During ablation surgery, the surgeon goes in and burns or lasers off the superficial portions of the endometrial lesions. The root of the lesions remains intact within the surrounding tissue. Excision surgery is oftentimes more expensive because of the expertise required to perform these surgeries. Remember, the surgeons performing excision surgery are more likely to be endo specialists which means this is what they deal with on a regular basis. These surgeons are more likely to understand and be able to identify areas of endometriosis. Endometrial lesions show up in a variety of colors, shapes, and sizes. The rate for repeat surgeries when excision was performed is significantly lower than ablation surgery. On average, individuals who undergo ablation surgery require a repeat surgery 2-3 years later.
- Pelvic Health Physical Therapy: Because of the tightening of muscles in response to pain, physical therapy is a great tool (or, dare I say, essential tool) in endo pain management. Finding a PT who is well versed in endo can be integral in helping manage GI dysfunction, fascial restrictions around the organs, nerve issues, pelvic floor tightening (in response to pain or related to intercourse), pain in low back and other body regions, and postural contributors.

- Diet: There is no ‘one size fits all’ diet when it comes to endo. It can take some time and experimentation to figure out what foods might be more inflammatory to an individual’s specific system. Some people may find their symptoms are helped by reducing or cutting out gluten, dairy, alcohol, soy, sugar, or red meat. Taking a food sensitivity test or discussing this with an endo specialist or dietician can be a great way to start getting an idea of what foods might have a negative effect.
- Stress: People can experience good stress and bad stress. Experiencing high levels of bad stress can contribute to inflammation in the body. Because endometriosis is an inflammatory disease, the goal is to reduce the amount of inflammation. Engaging in activities to de-stress will be important in caring for the mind and body. Examples may be painting, surfing, meditation, nature walks, dancing, playing music.

- Exercise: Movement is an important piece in managing endo symptoms. When someone is experiencing a flare, the go to position is fetal position or sitting. This static posture encourages blood to sit within the pelvic cavity with nowhere to go. Stagnant blood can contribute to pain so movement can help get blood flowing in and out of the pelvic region. This can look like stretching, yoga, running, hiking, biking, weight lifting, etc. What might work for one person may not work for another.
- Sleep: Good quality sleep can help the system heal, help with brain fog and fatigue, and decrease the brain’s perception of heightened pain levels.
- Supplementation: Modified citrus pectin, Quercetin, Omega 3, NAC, Curcumin, and Resveratrol are examples of supplements that research is showing can help reduce endometriosis pain, size and number of lesions.

- Medication: Orilissa is a medication that’s been out on the market for a number of years to combat endometriosis symptoms. This is a gonadotropin releasing hormone (Gnrh) receptor antagonist which is essentially blocking receptors to produce a drop in estrogen. It has helped many individuals with endometriosis but it has also been detrimental for others. Its side effects can be strong including menopausal symptoms like hot flashes, night sweats, bone loss, depression, and fatigue. As of Fall 2023, Myfembree has been approved for endo. It’s historically been used to treat uterine fibroids. Myfembree is also an Gnrh (same as Orilissa) but it’s combined with Estadial (estrogen) + progestin.
- Birth control: Can also be a helpful tool to manage symptoms but should be discussed with an endo specialist to decide on best forms of birth control to utilize.
- Acupuncture: Another great modality to help with stress and modulating the nervous system to help aid in pain management.
Let’s stop normalizing period pain. Endometriosis affects more individuals than we think and it’s likely we know of at least one person with it. If you think you have endometriosis, we encourage you to find an endo specialist who can help guide you in next steps. There are great resources online including Nancy’s Nook to find excision surgeons by state. If you’re looking for other resources to learn more about endo, please reach out to your nearest IPA Physio clinic and we can share those with you.