Could you have BPPV AKA Top Shelf or Positional Vertigo?
It is indeed likely as BPPV, or benign paroxysmal positional vertigo is the most common disorder of the vestibular system. It has an incidence of 107/100,000 per year according to Froehling DA, Silverstein MD, Mohr DN, et al.
BPPV is a non life-threatening transient vertigo dependent on head position and movement. Most cases are idiopathic; however, there has been correlation with trauma, migraine, inner ear infection, diabetes, osteoporosis, intubation, reduced blood flow, and sustained head position.
So what exactly is BPPV?
Within your inner ear, lies two adjacent structures; cochlea which you use for hearing sound and your vestibular apparatus which you use for balance. It is about the size of a dime and is made up of 3 semicircular canals and 2 pockets called the utricle and the saccule. The utricle houses calcium carbonate crystals called otoconia or otoliths (some people call these crystals).

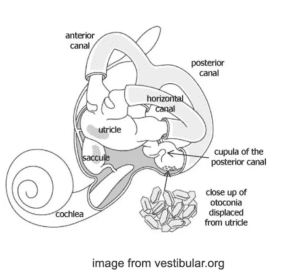
BPPV occurs when these otoconia or ‘crystals’ become dislodged and end up in the canals. When we move our head the fluid in the canals normally moves a little bit. When the otoconia are in one or more of the 3 semicircular canals, gravity acts on the otoconia which in turn moves the fluid more than usual. The brain receives a signal that produces a sense of motion which is inaccurate. This information does not correlate with information collected from the vestibular apparatus on the other side of the head, our muscles and joints in our neck, nor with information the eyes are providing. The spinning sensation is the result of mismatching information. Suffers of BPPV are sometimes asymptomatic between attacks when in non provoking movement or positions, while others have a milder version of the symptoms mentioned above even without movement.
BPPV will not:
- give you constant dizziness that is unaffected by position
- cause hearing loss or fainting feeling
- cause headache, numbness or other neurological symptoms (pins/needles/trouble speaking/change in coordination)
These symptoms need to be further evaluated by a physician and discussed with your PT as another possible vestibular disorder.
The Medical University of South Carolina has a helpful video to describe what is going on (link below).
MUSC: Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is diagnosed with a series of positional tests. This is sometimes done in the office of a Neurologist or ENT. More often, it is the Physical Therapist who has the time and expertise to test and immediately implement treatment.
There are 3 semicircular canals on each side which need to be assessed in addition to observation of eye movement. A test which confirms the presence of BPPV will provoke symptoms and show what is called nystagmus. This is a quick movement of the eye with a rebound which repeats for the duration that the otoconia are moving. The direction and length of time of the nystagmus will also give the examiner information about which treatment technique to then implement.
There are 2 types of BPPV:
- Canalithiasis
- otoconia are moving within a canal
- when movement stops the otoconia stop moving
- Vertigo and nystagmus cease in less than a minute
- Cupulolithiasis
- otoconia are located at the bundle of sensory nerves at the base of the canal
- vertigo lasts until the head is moved out of the provocative position
These types then have sub variants based on which canal is involved and if multiple canals are involved.
Treatment Options
Medications such as Bonine (meclizine) or dimenhydrinate(Dramimine) are often prescribed for vertigo, however this will not correct or treat BPPV, instead it dampens the symptoms such as nausea. In fact, if taken long term, it can result in other issues of the vestibular system.
The majority of cases are treated with mechanical maneuvers. These are called canalith repositioning maneuvers (CRMs). I like to explain this to my patients as using those old handheld mazes with a small bearing and you use gravity to move the bearing through the maze.
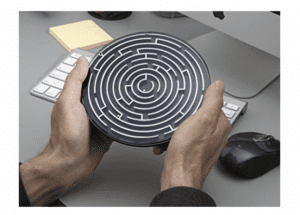

The head and body need to be moved in certain directions to use gravity to guide the otoconia back to the utricle. Depending on how chronic the BPPV is, this maneuver needs to be done multiple times. It is like a pile of sand in the gutter and there needs to be multiple passes of water for the sand to dissipate.
After treatment the risk for recurrence can be as high as 50% in the next 5 years according to Fife TD, et al.
Oftentimes those who have frequent recurrence learn CRMs from a trained practitioner and apply what is taught to them, correcting their own condition.There is some risk with just following YouTube videos if you have not been fully evaluated by a Physician or Physical Therapist. There are types and variants of CRMs and if application of the incorrect maneuver is done it may complicate your presentation. The easiest way to have your dizziness addressed is to see a Physical Therapist who treats vestibular disorders.
Highlights:
- BPPV is the most common form of vertigo
- It involves otoconia or crystals being dislodged from the utricle into the semicircular canals
- Medication does not correct BPPV
- BPPV is very treatable with maneuvers called CRMs
- There is some risk of recurrence however you can be taught to treat yourself
References:
Froehling DA, Silverstein MD, Mohr DN, et al. Benign positional vertigo: incidence and prognosis in a population-based study in Olmsted County, Minnesota. Mayo Clin Proc 1991;66:596–601.
Fife TD, et al. Practice Parameter: Therapies for benign paroxysmal positional vertigo (an evidence-based review): Report on the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2008;70:2067-74.
Sheelah Woodhouse, BScPT. Benign Paroxysmal Positional Vertigo (BPPV). 2015 Vestibular Disorders Association. https://vestibular.org/wp-content/uploads/2012/03/Benign-Paroxysmal-Positional-Vertigo-BPPV_8_0.pdf
The American Academy of Otolaryngology-Head and Neck Surgery’s.
http://eguideline.guidelinecentral.com/i/789708-benign-paroxysmal-positional-vertigo/13?m4=