Sleep – the 5th Vital sign

Inherently we all recognize that sleeping is important to our health, however we often view sufficient sleep (7-9 hours per night for adults) as a luxury and equate reduced sleeping time with increased productivity. Attitudes toward sleep are shifting in the medical community as research continues to reveal that sleep is not a period of physiological inactivity but is rather a critical period of recovery that supports numerous life functions (Barnes 2015). Many healthcare institutions are now emphasizing quality sleep so much so that it is recommended that sleep be adopted as the 5th vital sign in addition to blood pressure, pulse, temperature and breathing rate.(Reeve, 2010).
Between 50-70 million adults in the United States experience chronic sleep disturbances and 62% experience sleep problems multiple nights per week. Costs associated with chronic insomnia are over $100 billion annually (Wickwire, 2016)! Wow, what an opportunity to save our country money and make ourselves healthier!
Cumulative effects of sleep deprivation: chronic pain, depression, anxiety disorders, immunological conditions, reduced cardiovascular health, and degenerative neurological conditions.
Think back to a time when you didn’t sleep well for few nights in row. Remember feeling depressed or anxious? Do you remember having elevated pain levels? Did you have attention deficits or have a hard time remembering/processing information? How about poor physical performance? These are the cumulative effects of sleep deprivation and, if sustained, elevates your risk for developing: chronic pain, depression, anxiety disorders, immunological conditions, reduced cardiovascular health, and degenerative neurological conditions such as Parkinson’s Disorder.
See the post Restore My Sleep, Restore My Health!, to view a variety of strategies to start improving your sleep habits.
Sleep and Pain
It is intuitive that sleep and pain are linked together. Pain is uncomfortable and if you are uncomfortable, it makes sense that you would have difficulty getting quality sleep. What you might not recognize is the flip side of this point of view that not sleeping well will make you more susceptible to having an amplified pain experience as well as increases the risk of developing and sustaining new pain conditions. People who are sleep deprived are tend to have more frequent and intense spontaneous pain events, a lower pain threshold and have increased pain sensitivity.
The literature is not clear on the exact mechanism of why sleep deprivation makes you more susceptible to having pain or why sleep deprived individuals rate their pain intensity higher than individuals who are getting quality sleep. It is understood that there is overlap of the neuroanatomy and physiological processes in the brainstem between the areas that control sleep and the areas that modulate the “warning signals” (nociception) coming up from the body.
Consider the brainstem to be the “gatekeeper” that determines how much information is allowed to be transmitted to higher brain centers. The higher brain regions receive information, associate the data with previous experiences, and then creates what it has learned to be the appropriate output. In the case of receiving warning signals from the body, typically the response is to create pain in order to motivate the conscious mind to protect the affected area.
Rather than blocking these signals… a louder volume of signals is allowed to travel higher in the brain…
There is consideration that these brainstem regions become impaired and alter how much of these warning signals from the body are allowed to pass through the gatekeeper. In the impaired state, rather than gatekeeper blocking these signals entirely or muffling the volume of these signals as it would in the normal state, a louder volume is allowed to travel higher in the brain increasing the perceived “noise” coming from the body.
As the volume gets louder, the perception of a threat increases and when the brain feels threatened, the natural response is to increase pain output. The net result is the affected areas become more painful!
Developing and Sustaining a Sleep Disorder
Sleep deprivation somehow alters the function of the gatekeeper. In the development of a sleep disorder, there is often a precipitating factor such as a medical condition, losing a job, a change in schedule or a death in the family. The precipitating factor alters the established sleep rhythm and sleep hygiene, initiating the sleep disorder. After the precipitating factor is eliminated, the associated changes in sleep hygiene, or the habits and practices that are necessary to obtain good nighttime restful sleep and maintain full daytime alertness, remain and continue to sustain the sleep disorder. See Figure 1.
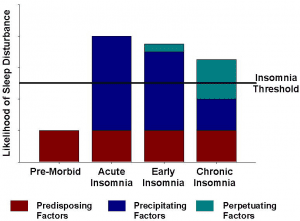
(Figure 1: adopted from Morin 2008)
Predisposing factors:
- anxiety
- depression
Precipitating factor:
- sudden change in life
- medication change
- injury
- schedule change
Perpetuating factors:
- poor sleep hygiene
- beliefs/thoughts/fears of sleeplessness
A common scenario is an injury changes your sleep patterns because you are simply uncomfortable in bed or wake up frequently because you are in pain. As a result, you start to take naps during the day, alter your eating habits or consume more caffeine throughout the day. Frequently, this leads to spending more time in bed looking at the ceiling ruminating on the fact that you can’t sleep or even worse you start looking at a bright screen at night, stimulating your brain to stay awake longer.
Gradually your bed becomes associated with thinking, being active or even suffering rather than being associated with sleeping. The tissues may have healed after several weeks but now the changes in sleep hygiene are preventing you from returning to a healthy rhythm of sleeping keeping your body in state of disequilibrium. As the cycle persists, the gatekeeper gets less effective at doing its job and the previously injured regions start to feel more vulnerable or painful. Or, perhaps new pain conditions start to surface. Put that on top of the lethargy of being sleep deprived and the stress on all other systems of the body and you can see how things start to go in the wrong direction.
There is Hope!
The good news is that the solutions can be as simple as starting to restore your sleep and rewire your brain back to a more efficient state! The brain and nervous system is very adaptable if given the right information to work with. Understanding how the changes take place, why they take place and recognizing that sleep deprivation is a major contribution to your health problems is a good place to start. The recognition of the root of the problem should help you gain in the necessary perspective and motivation to take immediate steps towards addressing the issue. Just imagine how good it would feel to hurt less, have more energy, take less medication, lose weight and increase clarity of mind! Additional practical solutions will follow in the next several blog posts, so stay tuned! See post on Restore My Sleep, Restore My Health for simple tips for sleep hygiene.
Regardless of how it started, I hope it is clear that restoring sleep is a critical piece that we must prioritize early in the plan of care if we are going to help restore your function and quality of life. Getting you out pain is very important and we can help you with this using Functional Manual TherapyTM techniques, educating you on the nature of pain, the nature of the injury and how to set the injury up for successful resolution. People often start feeling better within the first visit. Amazing what a skilled set of hands, empowering education and a well thought out plan of care can do to set the mind at ease creating an environment for success! If you would like to learn more about IPA Physio and how we can help you Discover your Potential!®, contact your local IPA Physio provider.
References
| Charles M. Morin and Geneviève Belleville (2008), Scholarpedia, 3(4):3314. |