Pain is your body’s alarm system. It’s not just there to annoy you; it’s a signal—a warning that something isn’t quite right. Just like a smoke detector alerts you to a fire, pain is your body’s way of demanding attention. But what if the alarm won’t shut off?
Or worse, what if you don’t know what triggered it in the first place? This is where physical therapy comes in. By addressing the root cause of pain, rather than just silencing the alarm, Functional Manual Therapy helps restore function, mobility, and overall well-being.
At IPA Physio, we specialize in solving these mysteries. We don’t just look at pain as a physical problem—we dig deeper, recognizing that pain is often influenced by many factors, from your diet to your sleep, and even your mental and emotional health. Let’s dive into what might be fueling your pain and how we can work together to turn off the alarm.
Our physical therapy clinic locations:
Portland
Orange County
Dallas
Steamboat Springs
New York
Physical Therapy and Dysfunction: The Starting Point
When it comes to pain, the most obvious starting point is physical dysfunction. This could mean stiffness, weakness, or poor posture. Physical therapy plays a crucial role in identifying and addressing these dysfunctions to restore movement and reduce pain. Physical issues generally fall into three main categories:
- Mechanical Capacity Dysfunctions – These occur when your mobility is restricted. Tight joints or muscles that don’t move as they should can create strain in other areas, leading to pain.
- Neuromuscular Control Dysfunctions – Weakness or a lack of endurance in key muscles can cause your body to overcompensate, which often leads to discomfort.
- Motor Control Dysfunctions – Poor posture or inefficient movement patterns can put unnecessary stress on your body, creating a cycle of pain.
These physical components are critical to address, but they’re often just the tip of the iceberg.
What’s Beneath the Surface? Hidden Factors That Amplify Pain
Pain is rarely just physical. It’s influenced by a variety of hidden factors that can magnify its intensity and duration. For instance, have you ever considered how your diet impacts your pain? Inflammatory foods—like sugar, alcohol, and fried snacks—can make your body more sensitive to pain signals. On the other hand, a nutrient-rich diet, filled with anti-inflammatory foods, can help reduce discomfort and support recovery.
Nutritional deficiencies also play a role. Low levels of Vitamin D, magnesium, or B12 can leave your body vulnerable to inflammation, fatigue, and muscle pain, and make it harder for your body to recover from stressors and injury.
But it’s not just about what you eat. Environmental factors, like allergies to mold, dust, or pollen, can create a chronic inflammatory response in your body, exacerbating pain even if the source isn’t obvious. Similarly, poor sleep habits—such as consistently getting less than seven hours of rest—can impair your body’s ability to heal, leaving you stuck in a cycle of discomfort.
Stress, Trauma, and Emotional Health
Your mental and emotional health can have a profound effect on how you experience pain. Stress, anxiety, and depression can heighten your sensitivity to pain signals, turning minor aches into overwhelming discomfort. Additionally, a history of trauma—whether physical or emotional—can leave lasting scars that influence how your body reacts to stressors. Even medical trauma, such as a difficult surgery or feeling dismissed by healthcare providers, can contribute to ongoing pain. Another significant variable in mental and emotional health is the presence or lack of a supportive community.
Even your past experiences with pain can shape how you perceive it now. For instance, if you were taught to “walk it off” as a child, you might ignore pain until it becomes unbearable. Alternatively, if past pain experiences were met with fear or catastrophizing, you might now associate any discomfort with worst-case scenarios. These learned responses can make pain harder to manage and resolve.
The Role of Lifestyle in Pain Management
Pain doesn’t exist in isolation—it’s influenced by a web of biological, psychological, and social factors. Stressful environments, emotional struggles, and physical limitations all combine to create a unique pain experience for each individual.
Your lifestyle choices also influence how pain shows up in your life. If you’re overtraining—pushing your body to the limit without giving it enough time to recover—you’re more likely to experience pain from overworked tissues. On the flip side, a sedentary lifestyle can weaken muscles and joints, making you more susceptible to discomfort. Striking a balance between activity and recovery is key.
There is such an emphasis on the latest and greatest recovery tools, but the best recovery tool known to man is restful sleep. Consistently getting less than seven hours of sleep per night can set the stage for pain. Sleep is when your body repairs itself, and poor-quality rest can disrupt this process, leaving you more vulnerable to inflammation and discomfort.
Airway Health and Breathing Patterns
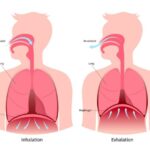
Breathing patterns are another often-overlooked factor. Shallow, chest-based breathing can increase tension in your neck and shoulders, while proper diaphragmatic breathing helps calm your nervous system and reduce pain. If you’re a habitual mouth breather or have a narrow airway, issues like sleep apnea could be silently contributing to chronic discomfort.
Your Body’s Pain Perception: More Than Just Physical
One fascinating aspect of pain is how some people are more in tune with their bodies than others. Those with a strong interoceptive sense (an awareness of internal bodily sensations) may notice and address pain early. Meanwhile, others might dismiss or overlook the signals until the pain becomes unbearable. This variability in body awareness can significantly influence pain perception and recovery.
Why Pain Is Like a Check Engine Light
Pain is a lot like the “check engine” light in your car—it’s a signal that action is needed to prevent further damage. The longer you ignore it, the worse the problem becomes. Addressing pain means looking at all the factors contributing to it and tackling them systematically.
At IPA Physio, we work with you to reduce the inputs contributing to your pain. By addressing physical issues, lifestyle factors, and emotional health, we help you turn down the “volume” on pain and restore balance to your body.
Pain doesn’t have to control your life. With the right approach, you can turn off the alarm and get back to doing what you love.

What Else Might Be Contributing to Your Pain?
There are numerous factors that can amplify discomfort or even cause it to linger. Here are a few:
Medications and Interactions
Certain medications can unintentionally make pain worse. Statins, fluoroquinolones, and opioids, for example, may have side effects that increase pain sensitivity or cause discomfort in unexpected ways.
Chronic Conditions
Autoimmune diseases like lupus, multiple sclerosis, Crohn’s disease, or rheumatoid arthritis can create persistent inflammation that heightens pain. Genetic factors, such as connective tissue disorders (like Ehlers-Danlos syndrome) or arthritic conditions, can also play a significant role in how your body perceives pain. Chronic infections and hormonal imbalances can further complicate the picture, making pain management feel like a never-ending battle.
IPA Physio – A Holistic Approach
At IPA Physio, we understand that pain is more than just a physical sensation—it’s a complex experience influenced by multiple factors. That’s why our physical therapists take a holistic approach, addressing not just the symptoms but the underlying causes of pain. Whether your discomfort stems from movement dysfunction, emotional stress, or environmental factors, physical therapy can help restore balance and function. Don’t let pain dictate your life—let IPA Physio guide you toward lasting relief and improved well-being.