Bowel movements. It’s something we can all relate to so I want to give you a quick and dirty run down of all things constipation. Most people suffer from constipation at some point in their life. This could be seasonal, when we travel, or on a daily basis. In the US, there’s an average of 2.5 million MD visits per year for constipation. That’s a lot of visits!
So how do you know if you’re constipated? Per Rome IV Criteria (the criteria used to diagnose constipation, Irritable Bowel Syndrome, as well as other GI tract issues), constipation is defined as having a bowel movement less than 3 times per week. Normal is considered anywhere from 3 times per day to 3 times per week. Although the criteria includes 3 times per week as the upper limit of normal, we believe that having at least one bowel movement per day is most optimal for the body. Having less than one bowel movement per day can have negative effects on your body including back and hip pain, abdominal and pelvic discomfort, cramping, bloating, uncontrollable gas, headaches, as well as increased stress on the GI tract. Chronic constipation can also result in hemorrhoids, anal fissures, rectal prolapse, and rectal bleeding if straining occurs during bowel movements.
The criteria states constipation must include at least two or more of the following: straining, lumpy or hard stools, sensation of incomplete evacuation, sensation of anorectal obstruction, and use of digital evacuation. With constipation, stools are typically hard, potentially small in size, and can be quite difficult to pass. When we experience constipation, we may also encounter bloating, passing gas, or abdominal pain.
Here are some potential causes of constipation:
 –Poor diet — Be sure to check that fiber intake! Aim for 25-30g of fiber each day. Think pears, avocados, strawberries, oats, lentils, chickpeas, kidney beans, almonds, chia seeds, kale, spinach, etc.
–Poor diet — Be sure to check that fiber intake! Aim for 25-30g of fiber each day. Think pears, avocados, strawberries, oats, lentils, chickpeas, kidney beans, almonds, chia seeds, kale, spinach, etc.
– Decreased water intake — Try adding in an extra cup of water every day for a week. If you normally drink five glasses of water a day, increase that to six glasses of water a day for the full week. Increase an additional cup of water daily each week until you find the amount of water that works for you to have more regular bowel movements.
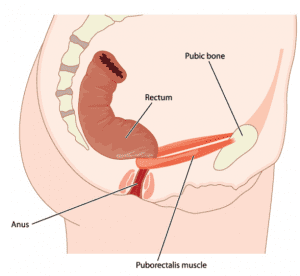
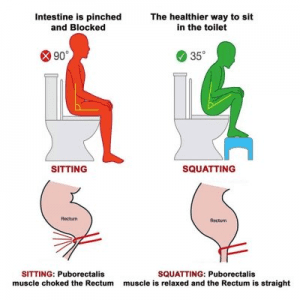 – Poor anorectal angle — When sitting upright, this creates a 90 degree angle of the trunk and upper legs. This particular position pulls on the puborectalis muscle and increases the angle of the rectum making it more difficult for stool to pass. By bringing the trunk forward and knees slightly higher, the puborectalis muscle becomes relaxed and the anorectal angle decreases which allows for a more direct and straight pathway for stool to travel. The Squatty Potty, as silly as it may sound, does help with bowel movements as it decreases the anorectal angle by bringing the knees above the hips which allows the puborectalis muscle to relax. Other ways of achieving this decrease in anorectal angle include lifting your heels up while leaning forward with forearms resting on the legs to improve the anorectal angle. Be mindful of toilet height as well. With a higher toilet seat, having something like a small step to bring the knees higher can be beneficial.
– Poor anorectal angle — When sitting upright, this creates a 90 degree angle of the trunk and upper legs. This particular position pulls on the puborectalis muscle and increases the angle of the rectum making it more difficult for stool to pass. By bringing the trunk forward and knees slightly higher, the puborectalis muscle becomes relaxed and the anorectal angle decreases which allows for a more direct and straight pathway for stool to travel. The Squatty Potty, as silly as it may sound, does help with bowel movements as it decreases the anorectal angle by bringing the knees above the hips which allows the puborectalis muscle to relax. Other ways of achieving this decrease in anorectal angle include lifting your heels up while leaning forward with forearms resting on the legs to improve the anorectal angle. Be mindful of toilet height as well. With a higher toilet seat, having something like a small step to bring the knees higher can be beneficial.
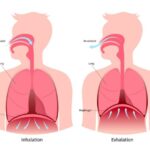
 – Abdominal hypoactivity & Diaphragmatic breathing — Diaphragmatic breathing is essential to keeping normal motility (capability to move, in this case, through the digestive tract). Oftentimes, people hold their abdominals tight and breath with their chest. This causes the diaphragm (which is part of the abdominal muscles) to become weaker as it’s not being utilized appropriately. This holding pattern can also lead to GI issues as tightness in the abdomen doesn’t allow the organs space to expand and relax as they need to move contents through your digestive tract. During bowel movements, diaphragmatic breathing and abdominal muscle activity are important to help move stool through the rectum and decrease risk of straining. Try taking a deep breath to expand your belly (diaphragmatic breath). While exhaling, harden your abdominal muscles as if someone were going to punch you in the gut. Continue with this cycle while trying to defecate. This encourages abdominal muscles to contract and help with motility of stool.
– Abdominal hypoactivity & Diaphragmatic breathing — Diaphragmatic breathing is essential to keeping normal motility (capability to move, in this case, through the digestive tract). Oftentimes, people hold their abdominals tight and breath with their chest. This causes the diaphragm (which is part of the abdominal muscles) to become weaker as it’s not being utilized appropriately. This holding pattern can also lead to GI issues as tightness in the abdomen doesn’t allow the organs space to expand and relax as they need to move contents through your digestive tract. During bowel movements, diaphragmatic breathing and abdominal muscle activity are important to help move stool through the rectum and decrease risk of straining. Try taking a deep breath to expand your belly (diaphragmatic breath). While exhaling, harden your abdominal muscles as if someone were going to punch you in the gut. Continue with this cycle while trying to defecate. This encourages abdominal muscles to contract and help with motility of stool.
– Muscle hyperactivity of the rectal pelvic floor muscles — These muscles need to relax, especially your puborectalis, to allow for a smooth pathway for stool to pass. Taking deep, diaphragmatic breaths as well as engaging in proper toilet posture can help relax this muscle. If the puborectalis muscle is in spasm, internal soft tissue work performed by a pelvic health physical therapist may be warranted.
– Paradoxical pelvic floor — Some people tighten their pelvic floor muscles during bowel movements without realizing it. Pelvic floor muscles and the internal and external anal sphincters should all be relaxing so stool can pass through the anal canal. Practice bearing down as if trying to have a bowel movement. The external anal sphincter typically contracts when trying to hold in gas. If it feels like the external anal sphincter is squeezing shut, it means these muscles are contracting instead of relaxing. If so, it means that there is a contraction of the muscles occurring rather than a relaxation.
 – Remember, medications can also cause constipation! — Opioids-narcotic pain medications, Calcium-channel blockers (high blood pressure medication), and antidepressants are all medications that may be contributing to your lack of consistent bowel movements. If you are constipated and on medications, it might be worth doing some quick research to see if a documented side effect is constipation.
– Remember, medications can also cause constipation! — Opioids-narcotic pain medications, Calcium-channel blockers (high blood pressure medication), and antidepressants are all medications that may be contributing to your lack of consistent bowel movements. If you are constipated and on medications, it might be worth doing some quick research to see if a documented side effect is constipation.
The Bristol Stool Scale is a great way to monitor what your stool looks like. As you can see, you want your stool looking like Type 3 and 4!

If you notice your stool is hard, try adding more water into your diet. This is a quick way to help improve ease of bowel movements without relying on medication. As mentioned earlier, taking small steps such as adding in another 8 ounces of water throughout the day for a week is an attainable way of increasing liquid intake. Continue adding an extra 8 ounces each week until you’ve reached the amount of water it takes to have easier bowel movements. If your stool is wet and loose, FiberCon and Citrucel can help add bulk. Psyllium Husk is another bulking agent that comes from plants. Appropriate water and food (specifically fiber) intake are the most ideal and sustainable for regular bowel movements.
Creating a routine for bowel movements is helpful for motility especially if there’s a tendency to feel constipated. A simple routine can include:
- Waking in the morning and having a warm beverage (coffee, hot tea, or warm water) to help push things along through the system. Coffee (because of the caffeine) as well as Smooth Move tea are great stimulators for motility in the colon.
- A colon massage can also be helpful to aid with colon transit time. The colon looks like an upside down U on your abdomen. Start on the left side of your abdomen underneath the rib cage and use gentle strokes in a downward motion.
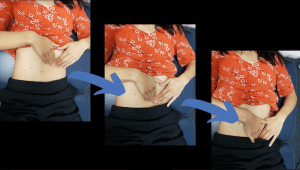
Move to the right side of the abdomen under the rib cage and move across the abdomen towards the left side and then down towards the left side of the pelvis.

Move to the bottom right of the abdomen and use gentle strokes up towards the right under side of the rib cage, across towards the left under side of the rib cage, and then down towards the left side of the pelvis.

Perform for 2-3 minutes.
- Gentle stretching such as the following can help stimulate movement throughout the colon:
- Supine Spinal Twist:


- Single Knee to Chest:


- Seated Spinal Twist:


- Child’s Pose:

- Try holding each position for 1-2 minutes while focusing on diaphragmatic breathing.
- Once you have the urge to have a bowel movement, go and don’t try to suppress it. If it doesn’t feel like the stool is going to come out, don’t sit on the toilet for longer than 5 minutes. People tend to strain and this can cause other issues including hemorrhoids, anal fissures, prolapse, and other pelvic floor muscle issues. Get up from the toilet and try out some of the stretches listed above, walk around the house, or massage your colon to aid in the movement of the stool.
And there you have it! Remember, pelvic health physical therapy can help with constipation. Besides providing some of the information listed above, a pelvic health physical therapist can help clue in on specific reasons why an individual is experiencing constipation whether it’s pelvic floor dysfunction or slowed colon transit time. Pooping is oh so important and if this is an area causing discomfort in your life, know that you are not alone and there are ways to improve this! For further questions, be sure to reach out to us at IPA Physio.
Bristol stool scale. (2021, January 02)
Rome IV Diagnostic Criteria for Constipation. (n.d.)